Genoptræning efter pectoralis major seneruptur
Title
Rehabilitation after a pectoralis major tendon repair
Topic
Rehabilitation, Musculoskeletal injuries
Authors
Camilla Holm Rasmussen, PT, Master of Science (MSc) in Physiotherapy
camilla.holm.rasmussen@regionh.dk
Bispebjerg og Frederiksberg Hospital
Publication date
Background
Pectoralis major tendon rupture is a rare injury first recorded in 1882 (1). The injury most commonly occurs in 20-40 years old male and have become more common because of the increasing popularity of bench pressing (1).
The pectoralis major is a powerful muscle that is responsible for abduction, flexion and internal rotation of the humerus (1). Patients often give a history of doing a maximal lift or effort and feeling a sharp tearing sensation and weakness in the affected shoulder, while the injury is often accompanied by an audible snap or pop (2).
Pectoralis major tendon repair is currently the recommended means of treatment (1). Treating this injury surgically is associated with lower incidence of strength deficiency and improved function compared to conservative treatment (3).
The conservative treatment is often recommended for less active patients who are having minimal pain or functional disability (3). This treatment consists of passive-assistive physiotherapy for three weeks followed by muscle strengthening exercises for several months (4).
In the clinical setting physiotherapeutic interventions are often used to store physical function and reduce pain after pectoralis major tendon repair, but the scientific background for the intervention are not clear. The purpose of this CAT is to systematically search and appraise the literature in order to elucidate the scientific background for applying physiotherapeutic intervention in the rehabilitation of patients with pectoralis major repair.
The clinical question
Is there any evidence for rehabilitation following a pectoralis major tendon repair?
Inclusion criteria
All articles on all levels of evidence involving rehabilitation after a pectoralis major tendon repair were included. The articles had to be written in English.
Exclusion criteria
Articles that solely were concerning surgery and surgical techniques
Search strategy
|
Patient |
Intervention |
|---|---|
|
Pectoralis major tendon [ti/ab] |
Rehabilitation [ti/ab] |
|
Pectoralis major tear [ti/ab] |
Rehabilitation [MeSH] |
|
Pectoralis major reconstruction [ti/ab] |
Early Ambulation [MeSH] |
|
Pectoralis major repair [ti/ab] |
Physical Therapy Modalities [ti/ab] |
|
Pectoralis major rupture [ti/ab] |
Physical Therapy Modalities [MeSH] |
|
Pectoralis major [ti/ab] |
Exercise protocol [ti/ab] |
|
Pectoralis muscles [ti/ab] |
Rehabilitation protocol [ti/ab] |
|
Pectoralis Muscles"[MeSH] |
Physical therapy [ti/ab] |
|
|
Physiotherapy [ti/ab] |
|
|
Physiotherapy specialty [MeSH] |
Figure 1: Search matrix
The terms in the patient and intervention category were combined with OR and afterward combined with AND. Medline, PEDro, Embase and Cochrane were searched and most recent search was dated March 20th 2020. Cinahl was out of order at that time.
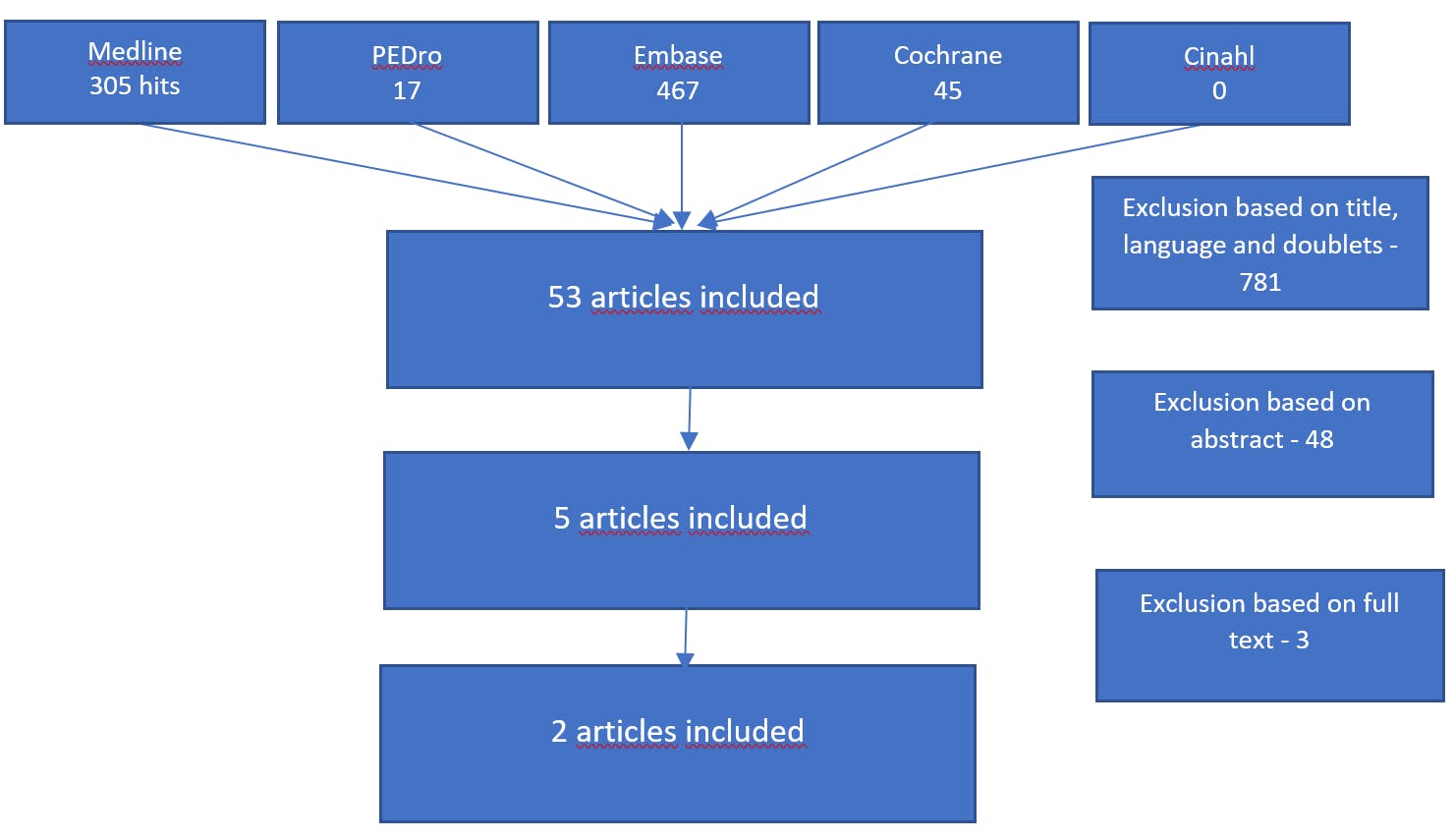
Figure 2: Flowchart
A total of 834 articles was found whereof 781 articles were excluded based on title, language and doublets, 48 were excluded based on abstract and 3 were excluded based on full text reading. Ultimately two articles were included for this CAT (figure 2).
No systematic reviews, randomized controlled trials or interventional studies investigating the purpose of this CAT were found, which led to two case reports were evaluated. There is no official checklist for case reports, but the CAse REport (CARE) guidelines (5) describe systematically reporting guidelines for case reports.
Critical evaluation
Vasiliadis, A. V. et al. 2016 (6):
Case report with one subject, a 30-year-old male with pain in his left shoulder after a fall while snowboarding. An MRI scan showed a complete rupture a few millimeters from the insertion on the humerus. The patient was treated surgically and afterward followed the rehabilitation protocol for Case 1 (Figure 3). The rehabilitation protocol lasted 16 weeks and had a gradually progression.
After the 16 weeks of rehabilitation, the patient gained full range of motion and was able to return to and participate in competitive contact sports.
Critical evaluation:
The authors have used this case report to present a rehabilitation exercise program and to suggest a reasonable schedule of activities of daily living and participation in sports after surgical treatment of a pectoralis major tendon rupture. The exercise intervention in this report is very well-described and therefore easy to reproduce.
According to the CARE guidelines (5), this case report lack a timeline in form of a table or figure giving the specific dates and times of important components of the case. The timeline should help give an overview of the key events of the case unfolded. Furthermore, no patient perspective or experience was described, which the CARE guidelines recommend.
Hoppes, C. W. et al. 2013 (7):
Case report with one subject, a 29 years old male serving in the US army in Iraq felt pain in the right shoulder after bench press. The patient was examined by a physician and referred to physiotherapy with the diagnosis: shoulder strain. The physical therapist examined the patient, who after sparring with two orthopedic surgeons got a MRI scan, that revealed a near-complete rupture. The patient was treated surgically and followed the rehabilitation protocol for Case 2 (Figure 3). The rehabilitation protocol lasted six months.
After 12 weeks the patient had full pain-free active range of motion and progressed well through the strengthening program in manner that allowed return to full duty. After six months the patient maintained resumption of full military duties and was performing a routine of strength training 3 times a week (a chest routine including dumbbell bench press with weight ranging from 11.3 to 15.9 kg and the ability to perform 50 push-ups without problems).
Critical evaluation:
The authors have used this case report to highlight the management of this injury within the unique constraints of combat environment. Even though this case report is special because of the environment, it is still transmissible to other patients because of how the injury occurred. The exercise intervention in this report is very well-described and therefore easy to reproduce.
According to the CARE guidelines (5), this case report lack a timeline in form of a table or figure giving the specific dates and times of important components of the case. The timeline should help give an overview of the key events of the case unfolded. Furthermore, no patient perspective or experience was described and whether the patient has given informed consent, even though it is recommended in the CARE guidelines.
|
|
Case 1 |
Case 2 |
|---|---|---|
|
Phase 1 (weeks 0-4 after surgery) |
Shoulder immobilizer worn at all times (except doing exercises) Elbow flexion and extension with the arm to the side close to the body (body in supine position) No further exercise |
No passive range of motion (PROM) Shoulder immobilizer worn at all times (except doing exercises) Hand-squeezing exercises with ball Elbow and wrist active range of motion (AROM) with shoulder in neutral position at side in an internally rotated/adducted position Stationary bike with immobilizer on, no weight bearing on involved under extremities (UE) Weeks 3-4 - Biceps curls and triceps extensions with light weight < 2.2 kg (arm at side) |
|
Phase 2 (weeks 5-6 after surgery) |
Shoulder immobilizer at all time Pendulum exercises - Arm side to side - Arm clockwise in small circles Self passive shoulder forward flexion up to 90 degrees
|
No PROM Shoulder immobilizer at all time (except during exercises) Shoulder shrugs, protraction, retraction, scapular mobilization Supine assisted active range of motion (AAROM) flexion to 90 degrees Submaximal multiplanar shoulder isometrics with elbow flexed 90 degrees and shoulder in neutral position at side Continue stationary bike |
|
Phase 3 (weeks 7-8 after surgery) |
Pendulum exercise after previous Self passive shoulder forward up to 90 degrees Abduction using wood ladder External rotation on table Internal rotation standing Flexion and abduction using physio ball Posterior scapular stretch Forward flexion with exercise bar |
No PROM Discontinue shoulder immobilizer Continue previous exercises AAROM flexion > 90 degrees AROM/AAROM in external rotation and abduction to tolerance Submaximal multiplanar shoulder isometrics Treadmill walking progression program |
|
Phase 4 (weeks 9-12 after surgery) |
Abduction using wood ladder External rotation on table Internal rotation standing Flexion and abduction using physio ball Posterior scapular stretch Flexion with exercise bar Pulleys in sitting position Biceps flexion with Thera-Band Triceps extension with Thera Band All of the above movement direction with Thera-Band Bent over row with Thera-Band Shoulder oscillation in abduction |
No PROM Continue appropriate previous exercises AROM, AAROM through full range Wall push-ups with a plus Bodyblade: Begin bilateral and progress to unilateral Ball toss with lightest ball (arm at side and chest pass) Elliptical trainer Treadmill jogging progression program |
|
Phase 5 (months 3-4 after surgery) |
Biceps flexion 7-10 kg Triceps extension 5-7.5 kg Forward shoulder flexion 5-6.25 kg Shoulder abduction 5-6.25 kg Shoulder adduction 5-6.25 kg Bent over row 10-15 kg Reverse fly 5-6.25 kg Wall push-ups Bench press 20-25 kg |
Continue appropriate previous exercises PROM as needed to regain full ROM Gentle pectoralis muscle stretches Shoulder internal and external rotation resistance training Biceps and triceps resistance training Begin upper-body workouts with very light resistance Upper-body ergometer 10 minutes forward and 10 minutes backward at low resistance Table push-ups Ball toss: Advance as tolerated Stairmaster Treadmill running progression program |
|
Phase 6 (months 5-6 after surgery) |
|
Continue appropriate previous exercises Knee push-ups à progress to regular push-ups Begin progression to heavier resistance upper-body workouts UE plyometric progression/sport specific drills/throwing progression Continue ROM restrictions on bench and pull-up (not > 90-degree elbow) Advance to outside running program |
Figure 3: Intervention protocol
Appraisal and conclusion
The purpose of this CAT was to investigate the evidence of physiotherapy rehabilitation following a pectoralis major tendon repair.
Even though the search resulted in 834 hits, most of the studies about pectoralis major tendon rupture investigated surgical versus conservative treatment and were often more than 10 years old.
No systematic reviews, randomized controlled trials or interventional studies with focus on the physiotherapeutic intervention on the rehabilitation were identified. Studies evaluating the physiotherapeutic intervention are still lacking and it was only possible to find two case reports that followed the physiotherapeutic intervention. The evidence level of the case report is very low, so the results are not transferrable to practice, but can still be used to generate hypotheses regarding the given treatment procedure.
No best practice for physiotherapeutic intervention on pectoralis major tendon rupture is described, but the case reports included showed some consensus in the rehabilitation protocols. The rehabilitation protocols are well described and therefor easy to re-produce.
The effect of physiotherapeutic intervention on rehabilitation after surgery for patients with pectoralis major tendon rupture remains to be elucidated and therefor interventional studies are needed on this topic.
References
1) Yu J, Zhang C, Horner N, Ayeni OR, Leroux T, Alolabi B, Khan M. Outcomes and Return to Sport after Pectoralis Major Tendon Repair: A Systematic Review. Sports Health. 2018; 11(2):134-41.
2) Bodendorfer BM. McCormick BP. Wang DX. Looney AM et al. Treatment of Pectoralis Major Tendon Tears – A systematic review and meta-analysis of operative and nonoperative treatment. The Orthopaedic Journal of Sports Medicine. 2020; 8(2): 1-14
3) Fleury AM. da Silva AC. de Castro Pochini A. Ejnisman B. de Lira CAB. dos Santos Andrade M. Isokinetic muscle assessment after treatment of pectoralis major muscle rupture using surgical or non-surgical procedures. Clinics. 2011; 66(2) 313-20.
4) Mooers BR. Westermann RW. Wolf BR. Outcomes following suture-anchor repair or pectoralis major tears: A case series and review of the literature. The Iowa Orthopaedic Journal. 2015; 35(8): 8-12
5) CARE – Case report guidelines [Internet]. Journal of Clinical Epidemiology. 2017. [cited 25 March 2020]. Available from: https://www.care-statement.org/checklist
6) Vasiliadis AV. Lampridis V. Georgiannos D. Bisbinas IG. Rehabilitation exercise program after surgical treatment of pectoralis major rupture. A case report. Physical Therapy in Sport. 2016; 20: 32-39
7) Hoppes CW. Ross MD. Moore JH. Undetected Pectoralis Major Tendon Rupture in a Patient Referred to a Physical Therapist in a Combat Environment: A Case Report. Physical Therapy. 2013; 93 (9): 1225-33.
Erklæring om forfatterens uafhængighed
Undertegnede erklærer at have følgende interessekonflikter i forhold til ovenstående CAT:
Fagpolitiske: Nej
Økonomiske: Nej
Du skal logge ind for at se kommentarer og selv kommentere
Log ind
Er du endnu ikke medlem? Bliv medlem i dag og få fuld adgang til fysio.dk, og gør brug af vores mange medlemsfordele.
