Therapeutic training intervention for Osgood-Schlatter disease
En CAT er et dynamisk redskab, som ikke har været igennem en videnskabelig bedømmelse. Derfor opfordrer vi alle til at kommentere, tilføje egne erfaringer og viden til den aktuelle CAT.
Topic
Rehabilitation
Musculoskeletal injuries
Sport
Authors
Rudi Neergaard Hansen, PT, MSc
rudi.hansen@regionh.dk
Mathilde Lundgaard-Nielsen, PT, BSc
mathilde.lundgaard-nielsen@regionh.dk
Bispebjerg og Frederiksberg Hospital
Fysio – og ergoterapiafdelingen
Publication date
15. December 2016
Background
Osgood-Schlatters disease (OSD) is the most common injury among children and adolescents who participate in sports activities (1, 2). OSD appears between the ages 8-14 in girls and between 10-15 in boys and the incidence is reported to be 21% of those actively participating in sports as compared with 4,5% in nonparticipants (3-6). Pain and tenderness at the tibial tubercle are the primary symptoms and OSD is typically a self-limited condition (1, 4, 5, 7). Recovery is expected for 90% of patients and symptoms are expected to extend through 12-24 months (3).
OSD is seen with activities requiring repeated knee extension whereby tensile forces pulls on the tibial tubercle apophysis. The ossification centre is unable to withstand these forces and bony or cartilaginous fragments follows (5, 6, 8).
Treatment is usually conservative and includes analgesics, ice, stretching, strengthening exercises and warm packs (1, 5, 6). About 90% of patients respond well to nonoperative treatment, but in rare cases surgical excision of the ossicle and/or free cartilaginous material is indicated (3). Even after treatment, some disability and insufficiency can persist into late adolescence and even adulthood (1, 9). On long term follow-up, 24% of patients have some limitation of activities, and 60% have discomfort with kneeling (10).
In the clinical setting exercise interventions are often used to restore pain and physical function, but the scientific background for the interventions are not clear. The purpose of this CAT is to systematically search and appraise the literature in order to elucidate the scientific background for applying training interventions in the treatment of Osgood-Schlatter disease.
The clinical question
What is the effect of therapeutic training intervention on pain and physical function in patients diagnosed with Osgood–Schlatter disease?
Inclusion criteria
We included articles of all evidence levels. There were no limits in publication dates. Article language was limited to Danish and English.
Only studies with a training intervention compared to no intervention or passive treatment were considered for inclusion.
Exclusion criteria
Articles that were solely concerning surgery and surgical techniques.
Search strategy
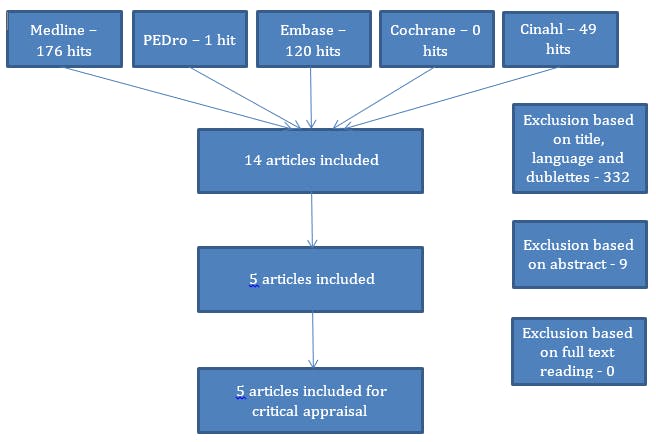
We searched Medline, PEDro, Embase, Cochrane and Cinahl. Most recent search was dated September 8th 2016.
We found 346 articles. 332 articles were excluded based on title, language and doublets, 9 were excluded based on abstract. 5 articles were ultimately included for this CAT (figure 1). After thoroughly reading these articles, we found no RCT’s or interventional studies. We decided to critically evaluate one article (11) using the AMSTAR checklist, since this review critically evaluated the literature. Furthermore we decided to make a summary and a critical evaluation of four reviews (3, 10, 12, 13) which provide an overview of the topic. These reviews content no critical appraisal of the literature and consequently we did not use AMSTAR.
One article (12) refers to a case series in which 19 of 24 knees demonstrated improvements in pain after using an infrapatellar strap (14). We also find referrals to other case series in which 88-90% of patients responded well to restriction of sports activity, use of nonsteroidal anti-inflammatory agents and/or cylinder casting (15, 16). It has not been possible to obtain these articles, but based on the description in the reviews, there is no training or exercise involved in the interventions, and they would therefore not be included in the appraisal anyhow.
Critical evaluation
Title: Evaluation and conservative treatment for Osgood-Schlatter disease: A critical review of the literature (11)
Purpose: To identify articles concerning diagnostic criteria and conservative treatment options for Osgood-Schlatter disease.
Study design: A critical review including 18 published studies from 1985 to 2013.
Methods: The authors of the review systematically searched the literature related to conservative intervention strategies in Osgood-Schlatter disease. The strength of evidence was assessed using an article classification table.
Results: 3 of the 18 studies included in the review were classified as systematic reviews, one study was classified as case series and the remaining articles were classified as expert opinion/commentary. There is strong evidence for conservative treatment including quadriceps and hamstrings stretching, quadriceps strengthening, ionophoresis and activity limitation.
Critical evaluation: After thoroughly reading the articles classified as systematic reviews and strong evidence, we find that the articles do not apply to the criteria defined in the Cochrane Handbook (17): They have no explicit purpose or intention to critically evaluate the literature, they contain no explicit search protocol and they summarise current evidence rather than appraise it systematically.
We have used the AMSTAR measurement tool to assess the methodological quality of the review and the score was 3/11.
Title: Osgood-Schlatter disease: review of literature and physical therapy management (13)
Purpose: Not specified.
Study design: Review
Methods: The review summarises the literature and physical therapy management.
Results: The primary concern is relief of pain in the area of the tubercle. The article recommends iontophoresis as initial treatment followed by stretching quadriceps and/or hamstring, and strengthening exercises. The article emphasises that patient and parent education with a reassurance that the condition is temporary, is a central part of the rehabilitation.
Critical evaluation: The article reviews histology, diagnosis and conventional treatment for Osgood-Schlatter but contains no systematic appraisal of the literature included. We consider the evidence level very low.
Title: What is the best treatment for Osgood-Schlatter disease?(12)
Purpose: Not specified.
Study design: Review
Methods: A small review describing the best treatment for OSD.
Results: OSD is best managed with activity modification, ice, anti-inflammatory agents, and time (since OSD is typically a self-limited condition).
Critical evaluation: The article contains no systematic appraisal of the literature included.
It gives a short description of common treatment modalities but has no value in appraising the current evidence. We consider the evidence level very low.
Title: Osgood Schlatter syndrome. Current opinion in pediatrics (3)
Purpose: The article provides a critical review of the current literature concerning diagnostic and treatment guidelines.
Study design: Review
Methods: The article describes best practice for treatment but emphasizes that they find no prospective, randomised, controlled, interventional studies to support the guidelines.
Results: The standard non-operative treatment of OSD includes application of ice, limitation of activities, oral anti-inflammatory medications, protective knee padding and physical therapy. The article recommends physical therapy including exercises for strengthening and improving flexibility of the surrounding musculature.
Critical evaluation: The article provides no description of the literature search procedure and it is therefore unclear to what extend the search has been comprehensive. We consider the evidence level very low.
Title: Osgood-Schlatter Disease (10)
Purpose: Not specified.
Study design: Review
Methods: The article reviews diagnosis, differential diagnosis and treatment for OSD.
Results: The article recommends patient information, short-term rest from the offending activities, knee sleeves and shock-absorbent insoles in mild cases. In severe cases periods of immobilisation with a cast or brace might be indicated.
Critical evaluation: The article contains no systematic appraisal of the literature included. We consider the evidence level very low.
Appraisal and conclusion
OSD is a common condition among adolescents and is quite well described in the literature, but studies evaluating the effect of therapeutic training interventions are still lacking. This CAT identified five critical reviews of which one article provides a systematic appraisal of the literature describing the procedure of the literature search. The four remaining reviews describe no literature search strategy and are best described as expert opinion/commentary.
Three of the articles described as systematic reviews in Kabiri L et al. 2014 (11) are in our opinion misclassified as strong evidence, resulting in an overestimation of the recommendations.
We identified no interventional studies that focus on therapeutic training interventions. Best practice in conservative treatment is generally described as ice, oral anti-inflammatory medications, activity modification, rest, protective knee padding and physical therapy including stretching of quadriceps and hamstrings and quadriceps strengthening exercises.
The effects of therapeutic training intervention for patients with OSD remains to be elucidated and therefore interventional studies are needed on this topic.
References
- Kaya DO, Toprak U, Baltaci G, Yosmaoglu B, Ozer H. Long-term functional and sonographic outcomes in Osgood-Schlatter disease. Knee surgery, sports traumatology, arthroscopy : official journal of the ESSKA. 2013;21(5):1131-9.
- Frush TJ, Lindenfeld TN. Peri-epiphyseal and Overuse Injuries in Adolescent Athletes. Sports Health. 2009;1(3):201-11.
- Gholve PA, Scher DM, Khakharia S, Widmann RF, Green DW. Osgood Schlatter syndrome. Current opinion in pediatrics. 2007;19(1):44-50.
- Cassas KJ, Cassettari-Wayhs A. Childhood and adolescent sports-related overuse injuries. American family physician. 2006;73(6):1014-22.
- Yen YM. Assessment and treatment of knee pain in the child and adolescent athlete. Pediatr Clin North Am. 2014;61(6):1155-73.
- Stein CJ, Micheli LJ. Overuse injuries in youth sports. The Physician and sportsmedicine. 2010;38(2):102-8.
- Launay F. Sports-related overuse injuries in children. Orthopaedics & traumatology, surgery & research : OTSR. 2015;101(1 Suppl):S139-47.
- Kaeding CC, Whitehead R. Musculoskeletal injuries in adolescents. Primary care. 1998;25(1):211-23.
- Maffulli N, Longo UG, Spiezia F, Denaro V. Sports injuries in young athletes: long-term outcome and prevention strategies. The Physician and sportsmedicine. 2010;38(2):29-34.
- Wall E. Osgood-Schlatter Disease. 1998.
- Kabiri L, Tapley H, Tapley S. Evaluation and conservative treatment for Osgood-Schlatter disease: A critical review of the literature. 2014;21.
- Bloom O. What is the best treatment for Osgood-Schlatter disease? 2004.
- Antich TJ, Brewster CE. Osgood-schlatter disease: review of literature and physical therapy management. The Journal of orthopaedic and sports physical therapy. 1985;7(1):5-10.
- Levine J, Kashyap S. A new conservative treatment of Osgood-Schlatter disease. Clinical orthopaedics and related research. 1981(158):126-8.
- Hussain AH, GA.; . Osgood-Schlatter disease. Sports Exer Injury. 1996;2:202-6.
- Mital MA, Matza RA, Cohen J. The so-called unresolved Osgood-Schlatter lesion: a concept based on fifteen surgically treated lesions. The Journal of bone and joint surgery American volume. 1980;62(5):732-9.
- Higgins JP. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0
Declaration of the authors independence
The authors report no conflicts of interest.
Du skal logge ind for at se kommentarer og selv kommentere
Log ind
Er du endnu ikke medlem? Bliv medlem i dag og få fuld adgang til fysio.dk, og gør brug af vores mange medlemsfordele.
